It kills bacteria in a new way
| THE INDEPENDENT | A new group of antibiotics with a unique approach to attacking bacteria has been discovered, making it a promising clinical candidate in the fight against antimicrobial resistance.
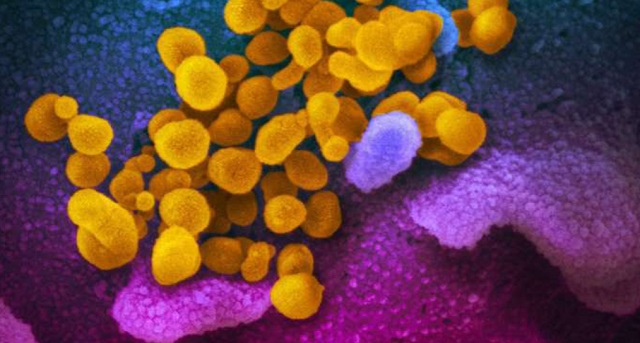
The newly-found corbomycin and the lesser-known complestatin have a never-before-seen way to kill bacteria, which is achieved by blocking the function of the bacterial cell wall. The discovery comes from a family of antibiotics called glycopeptides that are produced by soil bacteria.
According to the World Health Organisation, antibiotic resistance is one of the biggest threats to global health, with an estimated 700,000 deaths worldwide every year.
Corbomycin, along with a lesser-known antibiotic known as complestatin, kill bacteria by blocking the function of their cell wall, a phenomenon scientists have observed for the first time.
“Bacteria have a wall around the outside of their cells that gives them shape and is a source of strength,” said study first author Beth Culp, a PhD candidate in biochemistry and biomedical sciences at McMaster.
“Antibiotics like penicillin kill bacteria by preventing building of the wall, but the antibiotics that we found actually work by doing the opposite – they prevent the wall from being broken down.
“This is critical for cells to divide. In order for a cell to grow, it has to divide and expand.
“If you completely block the breakdown of the wall, it is like it is trapped in a prison, and can’t expand or grow.’
The researchers used a cell imaging technique to make their discovery. Culp said: “This approach can be applied to other antibiotics and help us discover new ones with different mechanisms of action”.
Both corbomycin and complestatin come from a family of antibiotics called glycopeptides that are produced by soil bacteria.
Tests on mice showed that these antibiotics can block infections caused by Staphylococcus aureus, a group of drug-resistant bacteria that can cause serious infections such as blood poisoning and toxic shock syndrome.
The researchers also demonstrated in mice that these new antibiotics can block infections caused by the drug resistant Staphylococcus aureus which is a group of bacteria that can cause many serious infections. The findings were published in `Nature’.
Looking at the family tree of known members of the glycopeptides, researchers studied the genes of those lacking known resistance mechanisms, with the idea they might be an antibiotic demonstrating a different way to attack bacteria.
“We hypothesized that if the genes that made these antibiotics were different, maybe the way they killed the bacteria was also different,” said Culp.
The group confirmed that the bacterial wall was the site of action of these new antibiotics using cell imaging techniques in collaboration with Yves Brun and his team from the Université de Montréal.
Culp said: “This approach can be applied to other antibiotics and help us discover new ones with different mechanisms of action. We found one completely new antibiotic in this study, but since then, we’ve found a few others in the same family that have this same new mechanism.”
The team is led by Prof. Gerry Wright of the David Braley Centre for Antibiotic Discovery within the Michael G. DeGroote Institute for Infectious Disease Research at McMaster.
The research was funded by the Canadian Institutes of Health Research and the Ontario Research Fund.
According to the World Health Organisation, antibiotic resistance is one of the biggest threats to global health, with an estimated 700,000 deaths worldwide every year.
Corbomycin, along with a lesser-known antibiotic known as complestatin, kill bacteria by blocking the function of their cell wall, a phenomenon scientists have observed for the first time.
What is antibiotic resistance?
Antibiotics have been doled out unnecessarily by hospital staff for decades, fueling once harmless bacteria to become superbugs.
The WHO has previously warned if nothing is done the world is heading for a ‘post-antibiotic’ era.
It claimed common infections, such as chlamydia, will become killers without immediate solutions to the growing crisis.
Bacteria can become drug resistant when people take incorrect doses of antibiotics or if they are given out unnecessarily.
Figures estimate that superbugs will kill 10 million people each year by 2050, with patients succumbing to once harmless bugs.
Around 700,000 people already die yearly due to drug-resistant infections including tuberculosis (TB), HIV and malaria across the world.
Concerns have repeatedly been raised that medicine will be taken back to the ‘dark ages’ if antibiotics are rendered ineffective in the coming years.
In addition to existing drugs becoming less effective, there have only been one or two new antibiotics developed in the last 30 years.
In September, the WHO warned antibiotics are ‘running out’ as a report found a ‘serious lack’ of new drugs in the development pipeline.
Without antibiotics, C-sections, cancer treatments and hip replacements will become incredibly ‘risky’, it was said at the time.
The findings stirred a positive response from other experts in the field.
Experts called the rising resistance to drugs a ‘major national and international concern’.
Despite excitement over the discovery, experts noted there is still a long and difficult road to generating an antibiotic that can be used in the clinic. Many new antibiotics fail clinical trials because they are found to be too toxic or not sufficiently effective when given to humans. There are also considerations of costs and testing for toxicity and efficacy in humans.
Of the many 1000s of promising new pharmaceutical compounds discovered or developed each year only very few actually get licensed after many years of further development and testing.
****
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



