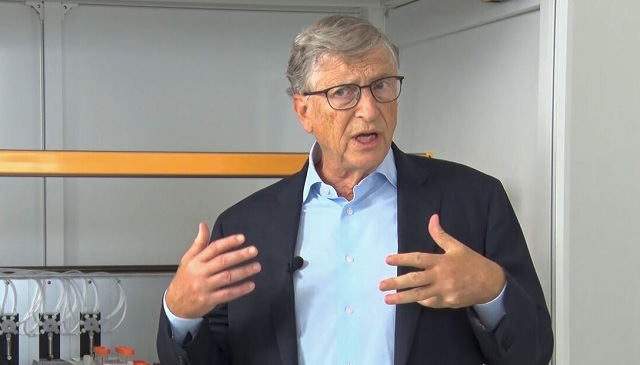
SPECIAL REPORT | THE INDEPENDENT | Philanthropist Bill Gates, the founder and co-chair of the Bill and Melinda Gates Foundation says more lives can be saved from HIV if modern HIV prevention tools can be spread out.
The Bill and Melinda Gates Foundation has been one of the biggest funder to HIV/AIDS research, treatment and lately prevention methods like preventative medications known as PrEP, or pre-exposure prophylaxis, which can reduce a person’s risk of contracting the virus by up to 99 percent when taken as prescribed.
” It’s an incredible feat of science: a pill that virtually prevents HIV contraction,” observes Bill Gates.
The foundation had by 2016 committed more than US$3 billion in HIV grants to organisations around the world and more than US$1.6 billion to the Global Fund to fight AIDS, tuberculosis and malaria.
As the world prepares to mark world AIDS Day on 1st December 2022 Bill Gates issued a statement on Tuesday saying that if we could get these tools to everyone who needs them and make sure they’re used correctly, we could stop HIV in its tracks. The problem is that countries like Uganda hardly provide funds in their budgets to make these prevention tools available as part of the fight against HIV. Activists like Lillian Mworeko, the Executive Director of International Community of Women With HIV(ICWL) its better to budget and provide funds for prevention of HIV than people being infected and require treatment for life.
“What is the cost of preventing a young girl from getting HIV and they are going to live the rest of their life fee of HIV? They are going to deliver babies free of HIV, and they are going contribute to the economy of their country. Compared to not acting now in the name of the cost and we are going to have this young person infected with HIV and we must treat them,” Mworeko asked.
Research on some of the available PrEP, or pre-exposure prophylaxis, that can reduce a person’s risk of contracting the virus by up to 99 percent when taken as prescribed were conducted in Uganda with the participation of Ugandan researchers including ordinary Ugandans forming part of the clinical trials.
These tools include the dapivirine vaginal ring (DPV-VR). The dapivirine vaginal ring or ring works by releasing the antiretroviral drug dapivirine from the ring into the vagina slowly over 28 days.
It protects the woman from HIV during sexual intercourse when used as recommended. The other tool prevention tool is the twice-annually injectable PrEP known as lenacapvir. Lenacapvir has been described a game changer in HIV prevention because it is closer to a vaccine. There is not yet a vaccine against HIV.
Trials for lenacapvir were also conducted in Uganda. The challenge is that all those prevention tools have not been widely circulated and there has been limited public outreach and information.
Bill Gates shares some of those concerns saying that even the most brilliant innovations make no difference unless they reach the people who need them most. “This is where partnerships become crucial,” he said
Bill Gates Full Statement
I’ve been working in global health for two and a half decades now, and the transformation in how we fight HIV/AIDS is one of the most remarkable achievements I’ve witnessed. (It’s second only to how vaccines have saved millions of children’s lives.)
At the dawn of the AIDS epidemic, an HIV diagnosis was often a death sentence. But in the years since, so much has changed. Today, not only do we have anti-retroviral medications that allow people with HIV to live full, healthy lives with undetectable viral loads—meaning they can’t transmit the virus to others. We also have powerful preventative medications known as PrEP, or pre-exposure prophylaxis, that can reduce a person’s risk of contracting the virus by up to 99 percent when taken as prescribed. It’s an incredible feat of science: a pill that virtually prevents HIV contraction.
In theory, if we could get these tools to everyone who needs them and make sure they’re used correctly, we could stop HIV in its tracks. Because when people with the virus receive proper treatment, they can’t transmit it to others. And when people at risk take PrEP, they can’t contract it. In practice, however, getting these tools to people—and making sure they’re used correctly—is the hard part. Especially for PrEP.
That’s because current preventatives require people to take medication every single day. Miss a dose, and protection drops. It’s like trying to remember to lock your front door 365 times a year—if you mess up once, you’re vulnerable. For many people, the barriers stack up quickly. Some have to walk hours to reach a clinic. Others struggle to store medication safely or discreetly at home. And many face judgment and stigma for taking PrEP, especially young women in conservative communities. The very act of protecting yourself can lead to being shamed or ostracized.
That’s why I’m so excited about a new wave of innovations in HIV prevention. Scientists are in the process of developing several longer-lasting PrEP breakthroughs, each with distinct advantages that could help more people protect themselves on their own terms.
Lenacapavir, which requires only two doses per year through injection, could open HIV prevention up to people who can’t make frequent clinic visits.
Cabotegravir, another injectable option that works for two months at a time, offers a more flexible dosing schedule than daily PrEP pills, too. Meanwhile, a monthly oral medication called MK-8572, still in the trial stage, could provide an alternative for people who prefer pills to injections. The Gates Foundation is even exploring ways to maintain a person’s protection for six months or longer. And researchers are working on promising PrEP options that include contraception, which would be particularly valuable for women who need both types of protection.
To understand how these options work in real life, and not just in labs, our foundation has supported implementation studies in South Africa, Malawi, and elsewhere. Unlike traditional clinical trials that test safety and efficacy in highly controlled settings, these studies examine how medications fit into people’s lives and work in everyday circumstances—looking at ease of use, cultural acceptance, and other practical challenges. This real-world understanding is crucial for successful adoption. Some people ask me if these new preventative tools mean the Gates Foundation has given up on finding an HIV vaccine. Not at all.
In fact, these advances push us to aim even higher in our research for a vaccine that could prevent HIV for a lifetime—and not just a few months at a time. Our goal is to create multiple layers of protection, much like modern cars have seatbelts, airbags, and even collision-warning sensors. Different tools work better for different people in different ways, and we need every tool we can get.
But even the most brilliant innovations make no difference unless they reach the people who need them most. This is where partnerships become crucial. Through grants to research institutions around the world, the foundation is working to lower manufacturing costs for HIV drugs so they’re accessible to everyone, everywhere. Then there are organizations like the Global Fund and PEPFAR, which have been instrumental in turning scientific advances into real-world impact.
The Global Fund—which needs to raise significant new resources next year to continue its work—currently helps more than 24 million people access HIV prevention and treatment. And PEPFAR has saved 25 million lives since its inception in 2003—a powerful example of how American leadership can build tremendous goodwill while transforming the world. Motivated by the belief that no person should die of HIV/AIDS when lifesaving medications are available, President George W. Bush created PEPFAR with strong bipartisan backing and it continues to serve as a lifeline to millions of people.
We’re at a pivotal moment in this fight. Twenty years ago, many believed it would be impossible to deliver HIV treatment at scale in Africa’s poorest regions. Since then, we’ve made fantastic progress. Science has shown us promising paths forward—for better prevention options, easier treatment regimens, and, maybe one day, an effective vaccine. Our task now? Ensuring the life-saving innovations we already have reach the people whose lives they can save.
*****
URN
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



