Trainee doctors are (barely) holding healthcare together
ANALYSIS | AGENCIES | As the Global North poaches African doctors, healthcare falls to overworked and unmentored interns, some of whom learn medical procedures from YouTube.
Fifteen of the world’s (fiscally) richest countries have over 55,000 African doctors in their health systems, a new data analysis by The Continent shows. These are doctors who qualified before entering those countries.
The United Kingdom is the top culprit, followed by the United States, France, Canada, Germany and Ireland, in that order.
Of the African countries being drained of doctors, an analysis of the latest data from the Organisation for Economic Cooperation and Development shows that Egypt has lost the most, followed by Nigeria, South Africa, Algeria and Sudan.
These countries have consequently paid a significant price in the quality of healthcare they can offer their own residents.
Egypt, for example, has the lowest doctor-to-patient ratio of its North African neighbours. In many of the drained countries, there are so few trained doctors left that the bulk of healthcare falls to doctors in training: medical interns.
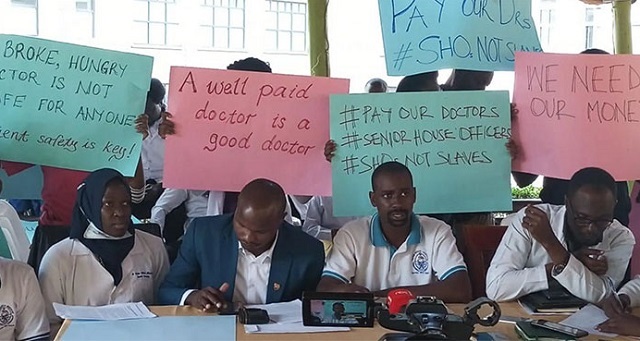
‘Treated like we are nobody’
Research in Uganda and Kenya details the cost to those interns. The study titled “We were treated like we are nobody” was published this November in the British Medical Journal for Global Health and is based on data on more than 700 medical interns in the two countries, as well as interviews with 54 junior doctors and 14 consultant physicians.
It found that medical interns are suffering from burnout and stress because they are working unreasonable hours and frequently don’t have superiors to train and supervise them. Their working conditions continue to have the same challenges that drive more experienced doctors to seek greener pastures.
The research found that the lack of support and supervision also “threatened individuals’ well-being and the quality of care being delivered”.
“Many reported working unreasonable hours – as long as 72 hours – due to staff shortage,” according to Yingxi Zhao, one of the researchers.
“Sometimes interns were the only staff managing the wards or had to perform certain procedures unsupervised. These included cases where interns had to learn how to perform Caesarean sections from YouTube.”
Threat to patients’ and doctors’ lives
Such conditions threaten not just the lives of patients but the trainee doctors too. Research by the World Health Organisation (WHO) found that people who work 55 or more hours a week had a 35% higher risk of suffering a stroke and a 17% higher risk of dying from ischemic heart disease, compared to those who worked 35-40 hours.
The Kenya and Uganda findings echo those of a Nigeria study published in May in the Public Library of Science journal.
Researchers interviewed 628 early career doctors and nearly 40% said they felt overwhelmed by their work. About 16% said they wanted to quit the profession and twice as many said they experienced anxiety.
The researchers in both studies recommend capping the hours that medical interns and junior doctors work. But limited training facilities and continuing brain drain make the doctor-to-patient ratio so low that reducing working hours is all but impossible.
By a large margin, the best doctor-to-patient ratios are in Libya and Algeria – 22 and 17 doctors for every 10,000 residents respectively. But even Libya and Algeria compare poorly to the top importers of African doctors, the UK and US, which have between 32 and 37 doctors for every 10,000 people.
To a doctor looking for a liveable work-life balance, going to the Global North is a no-brainer.
Lucy Nyokabi, a medical trainee at a Nairobi hospital, says her workload is overwhelming and she often doesn’t have safety equipment or the supplies to do the job properly, like oxygen masks.
“My family supports me in getting the things that I need for the job. I have to remind myself that I need this training to excel at the actual job,” she says.
This makes leaving attractive: “We all hope to work outside the country. I believe the conditions are better out there.”
*****
Source: The Continent
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



