Study looking at 200,000 young women finds no correlation
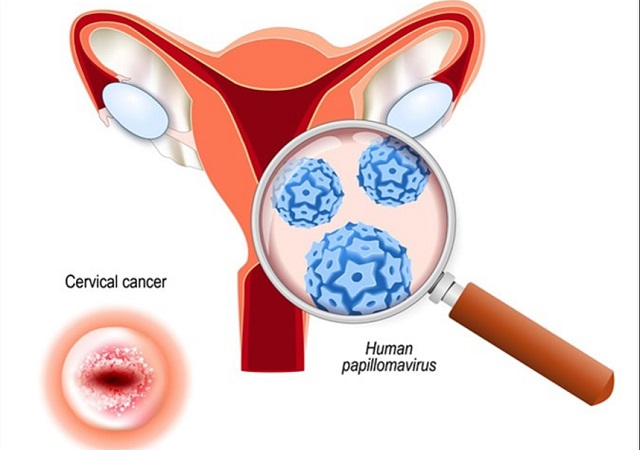
| THE INDEPENDENT | Human papillomavirus (HPV) is the most common sexually transmitted infection (STI). There are more than 100 Human papillomavirus (HPV) types that are transmitted sexually or via any skin-to-skin contact in the genital area.
Low-risk HPVs mainly cause wart formation on the genitals, anus, mouth, and throat, whereas high-risk HPVs, especially HPV 16 and HPV 18, are associated with HPV-related cancers. These viruses mainly affect the squamous cells that form the inner surface of various genital organs, causing a variety of HPV-related cancers, such as cervical cancer, anal cancer, penile cancer, vaginal cancer, and vulvar cancer.
After the initial approval of HPV vaccine in 2006 by the American Food and Drug Authority (FDA), there was public concern regarding the safety of the vaccine with particular focus on whether it could cause primary ovarian insufficiency or premature menopause. Too add to this concern, in 2014 a medical case report from Australia was published reporting three cases of unexplained premature ovarian failure in adolescent girls where an adverse reaction to Gardasil (HPV4) vaccination was hypothesised as a possible explanation.
New study
The author of a recent study analysing the National Health and Nutrition Examination Survey data on 8 million American women reported a correlation between women who had not had the vaccine and pregnancy.
At least 60% of women who did not receive HPV vaccine became pregnant at least once during the survey period (2007 – 2014), whereas only 35% of women who received the vaccine became pregnant. While the authors concluded that in an age group of 25 – 29 years, HPV vaccinated women are less likely to become pregnant than women who are not vaccinated, they have been roundly criticised for not taking into account the vaccine coverage in the respective age groups during the study period. Critics of the research have also pointed out that if the vaccine does affect fertility then a similar correlation would have been observed in other countries with good HPV vaccine coverage like Australia and the United Kingdom.
According to the data collected by the Vaccine Adverse Event Reporting System database, there were three reports of primary ovarian insufficiency out of 29 million doses of the Gardasil 9 HPV vaccine distributed in the United states between December 2014 and December 2017. All three were determined to be hearsay reports, meaning there was not enough information to confirm a medical diagnosis of primary ovarian insufficiency.
No correlation
The authors of recent study looking at 200,000 young women who received various adolescent vaccines including HPV vaccine found no correlation between HPV vaccination and increased risk of primary ovarian insufficiency. The researchers calculated that among 58,871 young women who received HPV vaccine, only one woman showed the symptoms of primary ovarian insufficiency, suggesting that HPV vaccine is unlikely to affect fertility in young women.
Infection with HPV affects reproductive health and fertility in both men and women. Particularly in men, HPV negatively affects various sperm parameters, including motility. The virus can also increase trophoblastic cell death and decrease the implantation of trophoblastic cells in the uterus. These factors can potentially increase the risk of miscarriage, premature membrane rupture, or spontaneous premature delivery.
In women undergoing intrauterine insemination, infection with HPV is associated with a lower pregnancy rate. In these circumstances it can be considered that a vaccine designed to prevent HPV infection should improve someone’s chances of having a successful pregnancy.
There is currently no reliable evidence that links current or previous HPV vaccines with fertility-related problems. However, given the questions raised by the case reports and recent academic controversy around the way large systematic reviews of HPV vaccine safety are conducted, it is clear that further research is needed to conclusively establish whether there are any grounds to associate HPV vaccination with any reduction in male or female fertility.
It is important to remember that a lot of studies on vaccine outcome reported that HPV vaccine is both safe and highly effective in preventing cancer-causing infections.
****
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price




Can you please link to the studies? It’s very hard to verify especially if we don’t know the qualifications of the author if this is even true. You don’t name the authors of the studies, the institutions, the locations…. please provide more data as this is an important topic. Conflicts of interest must also be stated. if you’re citing a CDC/Kaiser study well then they have a conflict as the CDC/HHS earns royalties on the HPV vaccine.