Sad situation leads to less-than-ideal healthcare service delivery system
Kampala, Uganda | THE INDEPENDENT | Healthcare worker strikes in Uganda are likely to have greater negative impact on poor and vulnerable patients, according to research published in Cureus, a journal of medical science which is part of Springer Nature; the German-British academic publishing company with headquarters in London, Berlin and New York City.
Services were paralysed in Uganda hospitals starting May 01 when pre-interns took to the streets to protest failure by the Ministry of Health to deploy them. This was the third time interns were striking in as many years over the same issues.
The nationwide strike followed an April 5 an announcement by the Minister of Health, Jane Ruth Aceng, that there would be a delayed deployment of the JHOs for the year 2023-2024. This was after a wait of over nine months for those who had completed final exams in May 2022.
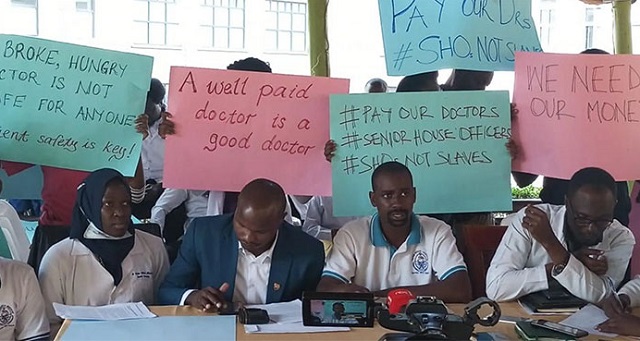
The government responded with force and many of the protesters were, according to the researchers, inhumanely treated and arrested by the Uganda Police Force. Meanwhile, the SHOs reactivated their industrial action and laid down their tools, and ceased working on May 1, 2023, over the payment of arrears.
On July 28, the Ministry of Health surrendered and cleared 1,901 medical pre-interns for deployment to 58 internship centers across the country. But there remains anxiety over their payment. The government in 2021 resolved that medical interns be paid a monthly allowance of Shs2.5 million with effect from July 01. However, the government says the newly deployed interns are to get only Shs1 million monthly.
Also, according to the researchers, the payment of monthly allowances of interns is frequently delayed, forcing many to live in harsh conditions. They may live in poor housing or be evicted from houses they rent. While hospitals in rural areas may be able to provide accommodations, over 100 interns living in the hostel of the national referral hospital were evicted for renovations in 2014. Interns in the public government hospitals always must find accommodation, food, and transportation, which is difficult when there is a delay or no payment. This has led to strikes in the past.
`Deserve Better pay’
“Medical workers deserve to be paid for their hard work, and appreciated for their performance, particularly in low-resource settings,” say the authors, doctors Esau Ogei and Catherine Lewis respectively of St. Joseph’s Hospital Kitovu in Uganda and East Tennessee State University, USA. Dr. Lewis is also a General Surgery practitioner at St. Joseph’s Hospital Kitovu.
Their research paper is entitled ` Medical Training in Uganda: A Critical but Neglected Part of the Healthcare System’. It offers a brief abstract of the structure of health care and facilities in Uganda, the role of medical students, interns, and medical officers, and their working conditions and pay. It also describes what it calls the “disruption in the fulfillment of basic health services” due to strikes.
“In order to prioritise the care of patients in the country, there should be fair treatment of the medical workers to boost and maintain morale and ultimately lead to continued quality patient care,” say the authors.
The researchers point out that healthcare worker strikes are not unique to Uganda and have become a growing concern to the international health community.
They say the inability of governments to deliver necessary healthcare quality and contribute to a better life for their citizens has led to healthcare worker strikes in low and middle-income countries such as Zimbabwe, Haiti, Kenya, South Africa, Nigeria, Sudan, and Uganda.
“Low pay or no pay has led to the majority of the strikes in Uganda,” they say. They say the World Health Organisation (WHO) mentions “a sufficient capacity of well-trained, motivated health workers” as a component of achieving universal health coverage.
The research paper is written under five main headings: Uganda’s healthcare system infrastructure, Medical education in Uganda, Nationwide strike by medical interns, Why medical interns strike, and consequences of the medical healthcare worker strike in Uganda.
The authors say quality healthcare is dependent upon the structure of healthcare and/or healthcare facilities in a country and that in Uganda, the healthcare system has had drastic changes over the last 50 years.
They point out that continuous demands for better working conditions and payment of arrears have forced the graduate medical students and upcoming medical interns to strike, causing disruption in the fulfillment of basic health services.
According to them, in the 1960s, Uganda had one of the best healthcare systems in East Africa. Hospitals were well-equipped, well-staffed, and had a set of connected healthcare units, they say. But political turmoil from 1970 to 1985 fragmented this healthcare system.
Today, although the Ministry of Health (MOH) is responsible for the majority of the healthcare services, the private sector and non-governmental organisations (NGOs) also play an important role. The study describes part of the hierarchy of Uganda’s healthcare system of health centers and hospitals that consist of seven levels. The study starts at Level V onwards.

Level V refers to general hospitals that are in each district. These have specialised clinics and consultants, and many are in the private sector. Level VI refers to regional referral hospitals that have specialised services and some residency programs. Currently, there is one level VII national referral hospital. This facility has advanced diagnostic services, advanced research capabilities, and “super-specialists. The authors point out that Uganda reintroduced free healthcare in the country in 2001.
A mandatory stage
The authors point out that supervised medical work or internship for one year is a mandatory stage for graduate medical doctors, pharmacists, dentists, and nurses before licensure. Under this arrangement, intern doctors, also known as junior house officers (JHOs), work with a provisional license under the supervision of senior medical doctors in the fields of surgery, internal medicine, pediatrics, and obstetrics and gynecology for one year. Thereafter, the new doctors are fully licensed by the Uganda Medical and Dental Practitioners Council (UMDPC).
At the time of doing the research, graduates who were waiting for internships (pre-interns) had finished their education about a year ago, in May 2022, but were still awaiting deployment by the Ministry of Health.
There is also another group called Senior house officers (SHOs) who are qualified medical doctors already registered and licensed by the UMDPC but are undergoing postgraduate training to become specialists in various fields of medicine.
These two groups, JHOs and SHOs, make up over 75% of the human resources for doctors in regional referral hospitals, national referral hospitals, and many private not-for-profit hospitals, and they are almost always the first responders. They deliver more than 90% of emergency obstetrics (childbirth and midwifery) care in regional and national referral hospitals where 78% of all maternal deaths occur.
Interns are oftentimes forced to work over 12 hours a day, seven days a week, without days off. The researchers say during the coronavirus disease 2019 (COVID-19) pandemic and the recent Ebola outbreak, many doctors worked long hours, were forced to quarantine, and sometimes worked without protective gear.
The payment of monthly allowances of JHOs and SHOs in Uganda is frequently delayed, forcing many to live in harsh conditions. They may live in poor housing or be evicted from houses they rent. While hospitals in rural areas may be able to provide accommodations, over 100 interns living in the hostel of the national referral hospital were evicted for renovations in 2014. Interns in the public government hospitals always must find accommodation, food, and transportation, which is difficult when there is a delay or no payment.
“Medical interns are supposed to be fully supervised by a senior consultant. However, oftentimes interns work more closely with medical officers or SHOs,” say the authors. They add that there is widespread absenteeism of senior consultants and a lack of oversight.
“That also causes the JHOs and SHOs to strike,” the research says. Medical officers have completed their internship but have not yet secured a spot as an SHO. They, therefore, do not have as much experience as the senior consultants.
Because of their tremendous contribution to the workforce, it was resolved that JHOs and SHOs would be paid a monthly allowance of Shs2.5 million with effect from July 1, 2021. However, these allowances are often not paid on time, and at the time of the research, there was a proposition to not pay these doctors at all. Meanwhile, the first-year SHOs had not yet received any government allowances, while the second and third-year SHOs have not been paid for about four to six months.
Later, an announcement was made that subsequently there would be no payment for their work and that those who could not pay their way through internship would therefore not receive their medical licenses. It was also said that the internship year would be considered a mandatory extra year for a medical degree, which is contrary to the current standard. The presentation of the MOH budget did not include JHO and SHO payments despite having had their monthly allowances raised less than two years ago.
The researchers say strikes have the potential to lead to either graduating doctors who are inadequately trained or, if there is prolonged delay in their training, the strikes could ultimately lead to a shortage of well-trained doctors as there will not be any new senior consultants who will enter the workforce. “Further delay may also cause many doctors to pursue training in other countries, leading to a shortage of physicians in Uganda,” they add, “Without the main source of healthcare providers, the country may experience increased mortality with the return of any outbreak or pandemic.”
“These endless strikes and issues of delayed deployment have always deterred service delivery in the regional and national referral hospitals, and even in private hospitals where interns train.” The researchers say, “Medical workers deserve to be paid for their hard work, and appreciated for their performance, particularly in low-resource settings. A boost in the morale of Uganda’s medical workers will ultimately lead to an overall improvement in the healthcare system.”
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price




A Society that fails to Recognize and Properly Renumerate it’s Health, Education and Security Sectors; the 3 major Foundations of that Society, is a Ghost Society, and is doomed to implosion.
Misguided Focus on Non Value Adding segments of the society such as the bloated legislature and the politicians therein, rather than those that keep society intact and moving forward is a sign of a government that doesn’t give a damn about it’s citizens. It’s a Ticking Timebomb.