But reducing poverty is the best way to end this disease
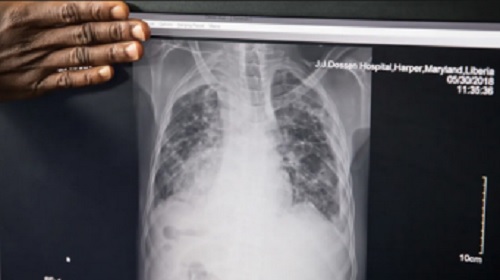
INTERVIEW | TOM NYIRENDA & NADINE DREYER | Every year, 10 million people fall ill with tuberculosis. Even though the disease is both preventable and curable, it kills 1.5 million people each year, making it the world’s deadliest infectious disease. Over 25% of these deaths occur in African countries. The World Health Organization has developed a strategy to reduce TB deaths by 95% by 2035. It’s a monumental task. But, global health and infectious disease specialist and Extraordinary Senior Lecture in the Department of Global Health, Stellenbosch University Tom Nyirenda, tells health editor Nadine Dreyer, there are grounds for hope.
Effective tuberculosis treatment has been available for decades. What makes it difficult to contain?
Tuberculosis is a disease of poverty. It thrives in poor living conditions and overcrowding. It’s a respiratory disease and spreads through the air when people cough, sneeze or spit. Victims need only to inhale a few germs to become infected.
In 1882, when the eminent German scientist Robert Koch discovered Mycobacterium tuberculosis, the microbe that causes tuberculosis, the disease sent shock waves throughout the world as it killed rich and poor alike.
At that time one in seven people in the US and Europe died from the “white plague”.
The Industrial Revolution had resulted in the urbanisation of the poor, who were forced into overcrowded, squalid conditions.
Housing conditions improved and by the time effective antibiotic treatments were discovered in the 1940s, TB rates in the west had declined.
In poor countries the vicious cycle of poverty and disease makes it difficult to eliminate TB. Poverty leads to poor health and unemployment.
Unemployment leads to poverty and poor health. There has however been progress in fighting TB in several African countries.
Tell us more about those countries and their successes
Last year the WHO reported that seven African countries – Eswatini, Kenya, Mozambique
South Sudan, Togo, Uganda and Zambia – had reduced TB deaths by a third since 2015.
The WHO’s Africa office identified several common strategies, all of which can be used by other countries on the continent and elsewhere in the world.
- Countries with limited resources need to choose where to concentrate them, for example, among people with HIV/AIDS who have a high risk of contracting TB.
- Educating healthcare workers and the public to recognise symptoms is key. These include persistent coughs, phlegm, weight loss, night sweats and high temperatures.
- The next step is to persuade the person suspected of having TB to get to a testing centre. There is a lot of stigma around TB, so this needs to be approached sensitively.
- Another challenge is making sure patients finish their medicine and get better. Treatment usually lasts for six months. There are some innovative ways to tackle this. For example roping in family members, community workers and even local neighbourhood shop owners to make sure patients take their pills. As human beings we can make things possible using our own communities. We have lots of solutions.
Have there been advances in TB treatment?
For many years it took three days to diagnose patients with TB. Three sputum smears were examined under a microscope to confirm the diagnosis.
Then, in 2001, there was a series of anthrax attacks on the US postal service. Powdered anthrax spores were deliberately put into letters that were mailed through the US postal system. Twenty-two people, including 12 mail handlers, got anthrax, and five died.
The molecular technology developed to detect anthrax revolutionised the diagnosis of tuberculosis.
The GeneXpert system, launched in 2003, was at the heart of biohazard detection for the United States Postal Service.
In 2010 the WHO gave the green light for GeneXpert to be used to diagnose TB.
The GeneXpert test can diagnose patients in an hour. A sputum sample is collected from the patient with suspected TB. The sputum is mixed with a reagent and a cartridge containing this mixture is placed in the GeneXpert machine. All processing from this point on is fully automated.
This was the first major breakthrough in tuberculosis diagnostics since the sputum smear microscopy was developed more than 100 years ago. Another big development is that for the first time in a century we are closer to an effective vaccine.
The BCG vaccine for TB has been used for 100 years. It is largely effective for children under five, but less so in older people and can’t be used on patients who have certain medical conditions.
The emergence of multidrug resistant forms of tuberculosis has increased the urgency of developing an effective vaccine.
There are 17 vaccine candidates currently in different stages of clinical trials. One of these is the M72 experimental vaccine. The late-stage trial of the vaccine is being rolled out in South Africa, Zambia, Malawi, Mozambique, Kenya, Indonesia and Vietnam. A total of 20,000 volunteers will take part in the trial, which is expected to run for five years. Medical advances are an essential tool to fight TB, but without combating poverty this devastating disease will remain with us.
*****
Source: The Conversation
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



