
Kampala, Uganda | RONALD MUSOKE | Even though the government has over the past couple of decades masterminded a wide-range of interventions in its fight against malaria, one of the deadliest diseases on earth, Uganda remains the third most affected country in the world according to data from the UN’s World Health Organization (WHO). Recent victims of the disease and some experts are blaming climate change for the explosion of populations of the malaria- causing mosquitoes in most parts of the country including colder areas like Kigezi in the Southwest, reports Ronald Musoke.
Mary Tibenkana, 28, a mother of three who lives in Mugona, a small village on the outskirts of Bugiri – a small town which is just about 150km to the east of Uganda’s capital city, Kampala, says it is difficult for anyone here to have a good night’s rest without sleeping under a mosquito net. She says the increase in mosquito populations in Bugiri District is disturbing.
“Even during day, mosquitoes bite,” she recently told The Independent. “I don’t know why this is the case; we just got mosquito treated nets and they just sprayed our houses (Indoor Residual Spray).”
She says residents have done everything the government has told them to do to prevent malaria but mosquito numbers and disease cases keep growing.
“We have been told to sleep under mosquito nets; we have been asked to clear bushes around our houses and to get rid of broken basins and used mineral water bottles that keep stagnant water. We have also been advised to report quickly to a government hospital when we fall sick so that we can get full treatment,” she told The Independent.
At Bugiri General Hospital which lies along the Iganga-Busia highway towards the Uganda-Kenya border, the Senior Assistant Nursing Officer and Malaria Focal Person at the health facility; Mary Nabwire, agrees. She says she gets bitten by mosquitoes in her home and even at her place of work.
“The mosquitoes are simply too many,” she says. When we recently met Nabwire, she told us she was recuperating following a recent bout of malaria. “I sleep under a mosquito net; my house was sprayed early this year but I got malaria last month (May) and I have just recovered. I have no idea where I picked it from.”
She suspects she could have picked it from the hospital’s Out Patient Department (OPD) where she sits from morning to evening to receive patients every day. She says Mondays and Tuesdays are the busiest days for the OPD. It is possible whoever fell sick on Friday, Saturday and Sunday waits for Monday to visit the hospital.
She opens her registry and lands on entries for Monday June 12. Of the 206 patients who visited the hospital that day, 39 turned out to be positive for malaria. But Nabwire says blood samples of 151 suspected malaria cases were sent to the laboratory for testing because the hospital does not take chances.
“Since this is like an epidemic, unless you come with an open wound, we normally test most of them who present with symptoms of malaria. Even if you come with cough, we will send you to the laboratory.” She says almost three quarters of those who are tested in the laboratory, their results are usually positive.
Bugiri District is probably the country’s epicentre of malaria at the moment. Even this year’s commemoration of World Malaria Day on April 25 was marked in Bugiri Municipality. The area offers probably the best example of what is at stake as Uganda tackles the increased malaria burden.
Nabwire says most patients at Bugiri Hospital’s Out Patient Department (OPD) present with malaria. She says they are in the thousands every month and include patients from surrounding districts of Busia, Mayuge, Bugweri, Namayingo and Namutumba.
“We don’t know whether it is because of the rainy season. May be the wet and warm conditions have made it a little more conducive for the mosquitoes to thrive here,” she says, “But it is also possible that the ever-rising human population has played a role; may be the more human blood the mosquitoes suck, the better their chances of growing and laying more eggs.”
Stubborn mosquitoes
What disturbs Nabwire and Tibenkana is that the malaria problem persists even when the government has provided a range of interventions to stop it. This includes recent distribution of free insecticide treated nets and indoor residual spraying (IRS). “After spraying, the mosquito population went down but they have since made a comeback,” Nabwire says.

Nabwire also told The Independent that although the government supplies the hospital with antimalarial drugs, they now suffer drug stock-outs. “What they (National Medical Stores) deliver gets finished very quickly, especially injectable anti-malarial medicine,” she says. She adds that the hospital also runs out of blood supplies needed to help patients with severe malaria who are anaemic.
There is no doubt that malaria is exerting pressure on the country’s health system with the government spending at least US$ 140 million every year to fight against the disease. The toll on drug stock, health workers and health facilities is also immensurable.
Nationwide malaria burden
Across the wider near eastern districts of Butebo, Budaka, Kibuku, Pallisa, Butaleja, Busia and Tororo, malaria cases have been on the rise. In Budaka District, the prevalence rate of malaria stands at 40% according to Dr. Erisa Mulwani, the District Health Officer. He says the upsurge in malaria cases has been consistent “for a long time.”
Dr. Mulwani attributes the high prevalence rate of malaria in Budaka to recent flooding of rivers and poor hygiene of the people. Not far away from Budaka, in Kibuku District, Rashid Kabaka Lubega, the Assistant in-charge of Kibuku Health Centre IV, the biggest health facility in this district, also complains about the malaria burden.
Lubega says the health facility is over-stretched with high malaria cases. He gives an example of the last quarter of the 2022/2023 financial year where the facility registered 4,778 malaria cases. “The facility is over stretched with high patient turn-up including patients trekking long distances to get treatment.”
Godfrey Buyinza, the Kibuku District Health Officer also told The Independent recently that according to their records, four in every 10 patients who present at health facilities in the district test positive for malaria. “The situation is quite worrying because the number of children dying as a result of malaria is quite alarming,” he said, “the disease has completely changed style because it sucks blood and leaves the children malnourished and anaemic.”
In the northern city of Gulu, malaria has also been wreaking havoc especially among children under five years old. Starting around October, last year, to May this year, Gulu Regional Referral Hospital registered over 6,800 cases of malaria with 72 people eventually succumbing to the disease.
The hospital receives patients from the entire Acholi sub-region in northern Uganda. At 36.5% prevalence rate among adults and 40.9% among children younger than five years, malaria remains one of the major killer diseases in the sub-region according to medical experts The Independent has talked to.
Dr. Paska Apiyo, the head of internal medicine at Gulu Regional Referral Hospital, however, told The Independent that more adults die of malaria at the regional referral than children and most of them are referred cases from nearby health facilities. She says the unavailability of rapid diagnostic test kits (RDTs) in smaller health facilities affects the timely examination of malaria patients.
At the nearby missionary health facility, St. Mary’s Hospital, Lacor, Dr. Godfrey Ojok, the Deputy Medical Director who also doubles as the in charge of community health services says the upsurge in malaria deaths in the sub-region is due to the delay of patients coming to the hospital to be properly diagnosed and treated.
Dr. Ojok told The Independent that the spike in malaria cases usually coincides with the wet season. He says the hospital is busiest during the months of February to May. “We usually have an upsurge in the admission cases of malaria and the situation stabilizes around June and July and again peaks in August when heavy rains resume again until October-November.”
While officiating at this year’s World Malaria Day in Bugiri under the theme, ‘Getting back on track through investing, innovating and implementation,’ Anifa Kawooya, the State Minister of Health in charge of General Duties, said the government is committed to increase its support to hospitals, increase drug stocks and other health supplies, and ramp up household indoor spraying of mosquitoes in affected communities.
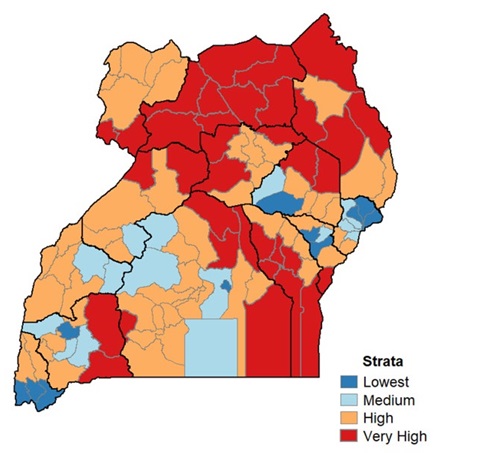
She said the Indoor Residual Spraying (IRS) programme would be ramped up in the most burdened regions of Acholi, Lango, Teso, Bukedi and now Busoga. But, the malaria-causing mosquitoes have been widening their range towards Uganda’s previously colder environs of Kigezi in southwestern Uganda and the Mt. Elgon region in the east of the country.
Malaria in Uganda’s highlands
David Ruzabarande, 70, a resident of Bigombe Road cell in Kabale Municipality in southwestern Uganda recently told The Independent that he first suffered from malaria when he was 28 years old in 1981. He caught the disease when he visited his relatives in present day Kamwenge District in Toro near the Rwenzori Mountains region.
“Being my first experience, I thought it was because of stagnant water we used to drink in trenches along the road to school. When I eventually visited a private clinic, the test confirmed that I had malaria,” he said
Back then, the Kigezi sub-region did not have mosquitoes and cases of malaria were rare. Ruzabarande told The Independent that he first heard about malaria in the 1960s from people who used to visit far away warmer provinces such as Toro and Buganda.
Today, malaria is quite common in Kigezi. Dr. Gilbert Arinaitwe Mateeka, the Kabale District Health Officer told The Independent that in 2022, the district recorded 1,277 malaria cases with one death. Dr. Mateeka says malaria cases were uncommon in the 1960s due to the unsuitable cold climate for mosquitoes.
“However, globalization, where people can easily travel to different districts within a single day, along with environmental encroachment and degradation, has contributed to the increased cases of malaria,” he says.
Still, Mateeka says, Kabale District typically experiences an upsurge in malaria cases after festive seasons such as Christmas and Easter, often transported from districts with higher malaria prevalence.
In the eastern highlands of Elgon, malaria has also picked up in recent decades. Dr. Yonas Oboth, the Hospital Administrator of Mbale Referral Hospital says they have been recording an average 700 malaria cases every month. But he says they recorded over 1,092 cases in May.
He says this year, they recorded the highest cases of malaria in January, February and March and attributes the increase to the weather. “We usually experience high cases of malaria during the rainy season and at the peak of drought and we can attribute it to changing weather patterns,” he said.
James Wamono, an environmental expert based in Mbale says malaria is becoming common in the Elgon region, especially in the rural areas, because the people have cut down trees and the place has become warmer.
“Global warming induced by human activities has increased the risk of vector-borne diseases such as malaria in Bugisu,” he told The Independent. Wamono’s attribution of the upsurge of malaria cases in Uganda’s cooler regions such as Elgon and Kigezi is supported by recent studies.
Should we blame climate change?
Interestingly, Dr. Jimmy Opigo, the Manager of the Malaria Programme at Uganda’s Ministry of Health told The Independent that Uganda is a malaria-endemic country meaning there is stable transmission.
“When you say there is an upsurge, it means the cases have risen above the expected number of cases but what we are experiencing is what is expected,” he said.
Dr. Opigo said large parts of Uganda have big swathes of surface water. Eastern Uganda, for example, which is currently burdened by malaria is drained by an expansive wetland around River Mpologoma to the east, Lake Kyoga to the north, Lake Victoria to the south and River Nile to the west with hundreds of tributaries and small streams crisscrossing the land.
This kind of environment is probably suitable for the Anopheles gambiae, one of the most aggressive malaria causing mosquitoes in Uganda. “Just like people consider Uganda to be the Pearl of Africa, it is the same for mosquitoes,” Dr. Opigo says.
But, what about malaria cases in colder parts of Uganda such as Kigezi in southwestern Uganda?
Dr. Opigo told The Independent that the answer is not as straight forward. Local research is also not as readily available to support or downplay the role of climate change in the nationwide burden of malaria.
However, in a paper published in The Lancet Planetary Health Journal in April, last year, the researchers found that the seasonality and spatial distribution of malaria cases are affected by climatic factors, particularly temperature, which affects the population dynamics and biting rates of mosquitoes that transmit the disease. Temperature also affects the sporogonic cycle of these mosquitoes.
The paper, “The relationship between rising temperatures and malaria incidence in Hainan, China, from 1984 to 2010: a longitudinal cohort study,” used a decades-long data set of malaria incidence reports from Hainan, China, to investigate the pattern of malaria transmission in Hainan relative to temperature and the incidence at increasing altitudes.
Another paper titled, “Climate change could shift disease burden from malaria to arboviruses in Africa,” which was published in the Lancet Planetary Health Journal in September, 2020, Dr. Erin A. Mordecai (PhD) and others argue that climate change will affect vector-borne disease transmission because changes in temperature affect vector population size, survival, biting, pathogen incubation rates, and vector competence.
Dr. Opigo explained to The Independent that: “Climate change or climate variability manifests in different ways; it can manifest in the rise or drop in temperatures. And we also know that mosquitoes need a certain level of temperature to breed but also for the parasites inside them to develop,” he told The Independent.
However, Dr. Opigo says, according to what they have observed over the last five years (relying on data from the Uganda National Meteorological Authority (UNMA), the minimum and maximum temperatures have remained within the range mosquitoes require to thrive.
But Dr. Opigo adds that since flooding episodes tend to destabilise communities by sweeping away their houses, the victims end up crowding into makeshift camps without proper housing, which is one of the most important malaria control measures.
“So, in this context, the effects of climate change (flooding) could have to do with population displacement and destabilization of their normal lifestyles,” he says.
Dr. Opigo adds that the other climate variability is drought. “Usually when there is prolonged drought, people become complacent and when mosquitoes breed in those areas following heavy rains, malaria cases shoot up,” he says.
Dr. Opigo further explains that climate change also tends to affect the way mosquitoes behave. “Mosquitoes live for only one month; so in one year there can be at least six generations. So, their genetic make-up and behaviour can be altered quite fast. They may, for instance, decide not to bite you inside your house, they may decide not to rest indoors,” he says.
“This is what we have observed in eastern Uganda. We deployed IRS but realized that nothing was happening. We later observed that mosquitoes are no longer dwelling inside the houses. We found the population of mosquitoes which can bite you from outside your house had increased relative to those which bite you while indoors.”
“For those which bite from inside people’s houses, we found that they had stopped resting on the walls (after biting you). They now bite and fly out of the houses. We are yet to find out the factors behind this change in behaviour but it can either be climate-change related or a reaction to the pressure the mosquitoes are feeling due to malaria control measures.”
Dr Jonathan Kayondo, a research biologist based at the Uganda Virus Research Institute (UVRI)’s Department of Entomology in Entebbe says this is not surprising. He told The Independent that mosquitoes are living things and also respond to the environmental pressure thrown at them.
Malaria and Poverty
Meanwhile, Dr. Opigo told The Independent that there is one other factor that should not be downplayed when it comes to malaria prevalence. He says there appears to be a correlation between high malaria incidence and level of poverty in the country. “If you get the Uganda Bureau of Statistics (UBOS) poverty map, it exactly overlays the regions with the highest malaria burden,” he said.
“And if you dig deeper, even within those malaria-prone regions, you will find that the urbanized areas have less malaria because housing is relatively better, drainage is fixed, people’s compounds are groomed and the residents have relatively better access to healthcare services.”
Opigo told The Independent that the people in urban areas also tend to be more educated than rural people, meaning they are more likely to adhere to malaria preventive measures than rural folk.
Interestingly this is what Mary Tibenkana says she and residents of Bugiri have been doing and yet they still have a malaria problem.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



