
The vaccine being introduced is being given to children between five and 15 months old
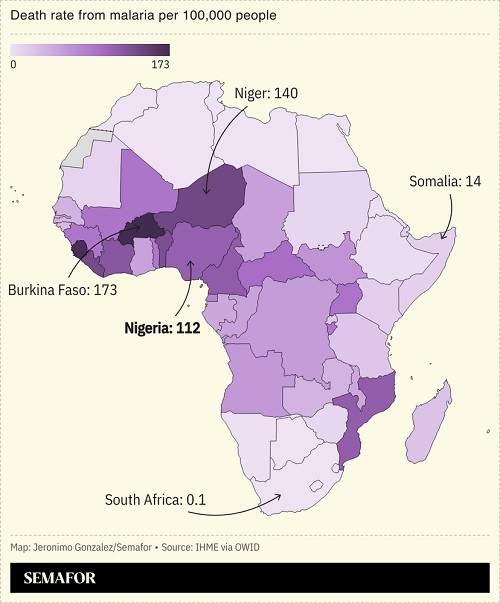
Nigeria | AGENCIES | Nigeria, which has more malaria deaths than any other country in the world, has begun rolling out a vaccine against the disease for the first time.
The West African nation accounts for almost a third of those who die from malaria each year.
The vaccine being introduced – called R21/Matrix-M – is the second to be approved by the World Health Organisation (WHO) and is being given to children between five and 15 months old.
Researchers say it is 75% effective but health experts recommend using it alongside other malaria prevention tools, such as mosquito nets and insecticides.
The roll-out started in two of the worst-affected states – Bayelsa and Kebbi – and the plan is to expand it to the rest of the country by next year.
Happiness Idia-Wilson’s 11-month-old son was the first to receive the vaccine at a ceremony in Bayelsa.
She said she was doing it “for the safety of the child, for him to be protected”.
“I will tell mothers, and I will invite people (to be vaccinated),” the mother added.
Bayelsa’s commissioner for health, Prof Seiyefa Brisibe, said the state would be carrying out health campaigns to promote the use of the vaccine in all the local languages.
In 2022, Nigeria accounted for 27% of global malaria cases and 31% of malaria deaths, according to the WHO, with children under five and pregnant women being the most vulnerable.
Africa overall saw 95% of those deaths, amounting to some 580,000 people.
“We are confident that this vaccine, in combination with other preventive measures, will drastically reduce the burden of malaria in Nigeria and help us move closer to achieving the goal of a malaria-free Africa,” said Dr Walter Mulombo, WHO representative in Nigeria.
The government estimates that Nigeria loses $1.1bn (£870m) each year due to lost productivity and health expenditure linked to malaria.
The Nigerian government took their first delivery of malaria vaccines in October 2024. Designed to bolster already implemented interventions like the distribution of insecticide-treated nets to households, over 800,000 doses are expected to be distributed during this initial phase.
Nigeria’s Minister of Health and Social Welfare, Prof Ali Pate, while receiving the vaccines in Abuja last month, said that the arrival of the malaria vaccine was a huge step in the country’s effort to reduce malaria cases and related deaths.
“With the support of UNICEF, Gavi and WHO, we are on a path toward achieving our goal of a malaria-free Nigeria,” he said during the occasion.
While the arrival of the preventive vaccine has offered some relief and hope to parents in parts of the country, in Bayelsa, one of the two states where the first roll-out will take place this month, some mothers wished the vaccine had come earlier.
“My second child suffered from frequent malaria, and unfortunately I didn’t know about it on time until she died. My baby is five months old now, and I would like to give him the vaccine to protect him. The vaccine will be very helpful for us because many children die due to malaria,” Permanent Epiere, a mother of two in Onuebum community under Ogbia council area of the state, told VaccinesWork.
Prof Mokuolu sees a ray of hope with the arrival of the new vaccine. He believes that the roll-out will lead to reduced hospital visits for children and increase survival rates for those within the most endangered age bracket.
“The malaria vaccine offers an immense opportunity as an added tool to the fight against malaria,” he said.
R21/Matrix-M, developed by the Jenner Institute at Oxford University, uses three doses administered four weeks apart and a booster dose given after one year.
Earlier this year, Ivory Coast and the Democratic Republic of Congo also began using the vaccine. Ghana, Kenya and Malawi have trialled another malaria vaccine – RTS,S. Nigeria was not included in the subsequent roll-out of the jab by the WHO to 12 African countries.
Nigeria’s malaria frontline
Single mother of twin boys Kelechi Ukatu is familiar with the pain and nightmare that malaria brings. Since she gave birth to her children, the parasitic disease has ensured that she knows only little sleep. Day and night, at different times, malaria has infected her boys, leaving her to contend with a heavy burden.
Apart from the resources that go into seeking treatment each time they fall sick from malaria, the psychological trauma that comes along can be devastating.
“There have been occasions when we are forced to wake up in the middle of the night to rush the children to the hospital because of malaria. We have become frequent visitors to different hospitals because of this situation,” Ukatu says.
Aina Ogundare is also familiar with the pain and nightmare that malaria brings.
“I cannot afford to lose her,” she vowed recently as she tightly clutched her crying three-year-old baby, Tunmise, as she waited to see a doctor at the Ikorodu General Hospital.
“I will do anything I can to ensure she overcomes this sickness,” the young mother said as a nurse tried to calm her fears.
Looking visibly worried and ruffled, the 34-year-old was surrounded by dozens of other women who had defied an early morning downpour to besiege this Lagos hospital in search of medical care for their loved ones. Laboratory test results confirmed that the little girl had malaria.
Ogundare has valid reasons for expressing such worry. Four years ago, she lost her only child at the time, Ayomide, to malaria.
Though the arrival of Tunmise helped reduce the impact of that loss, the constant threat posed by malaria has ensured that the shadow of that tragedy continues to lurk.
“I cannot count the number of times that my baby has fallen ill to malaria,” Ogundare told VaccinesWork as she walked out of one of the three consultation rooms on the ground floor of the hospital.
“The situation has drained our resources and taken a huge mental toll on us,” she added, before heading to the dispensary to purchase prescribed drugs for her daughter.
The impact of conflict
In other parts of Nigeria, especially in the northeastern region, where conflict has sacked communities and forced families to take refuge in camps, the threat and danger posed by malaria remain real and severe.
In Borno, one of the six states in the region and epicentre of the insurgency that has left behind a full-blown humanitarian crisis, malaria spares no one. Young and old have been left to contend with a ruthless killer.
“My neighbour lost a child to malaria in September after floods overran our community,” Aisha Aliyu, a mother of one living in Maiduguri, Borno’s capital, recalls.
“Less than a week after that incident, my son, Ali, also fell ill from the same disease. I was confused and afraid that I was going to lose him.
“Though he is well now, he has not been the same child again, especially since we don’t have a treated net to protect him from mosquitoes,” she added during an interview with VaccinesWork.
Fatima Hassan, who also resides in the same city with her daughters, lost a nephew to malaria two years ago. Following a rise in malaria cases in her neighbourhood since September, after floodwater from a collapsed dam overran parts of the region, she has grown worried for the safety of her girls.
“The threat of malaria in this part of the country has increased over the last two months. The situation has exposed our children to the disease, and this is affecting our lives a lot.
“We hope that the authorities do something about this problem soon, before we lose more lives to malaria,” she said.
Nigeria’s malaria burden
Saliu Ibrahim, a medical doctor in Kebbi, the state with the highest malaria prevalence in the country, said that nearly eight in every ten cases attended to at the government facility where he works is malaria-related. He fears for the worst if urgent measures are not taken to tackle the situation.
“As medical personnel, we are mostly overwhelmed as a result of the number of malaria cases we attend to every day. The number of casualties related to the diseases makes it a serious crisis that must be quickly looked into by higher authorities,” he said.
The leading cause of death among children five years and below as well as pregnant women in Nigeria, malaria continues to wreak havoc across the country, inflicting households and entire communities with wounds that may never fully heal.
WHO’s 2023 World Malaria Report reports that Nigeria accounted for 27% of the global malaria burden – the highest in the world – with a national prevalence rate of 22% in children five years and below. In the northeast region, the figure is as high as 49%.
Transmitted to humans by female Anopheles mosquitoes, malaria is a common fixture all year round in the country, especially during the rainy season when the flooding of communities encourages disease spread. Health authorities put the economic burden of the disease on Nigeria at US$ 1.6 billion annually, pointing out that the amount could rise to US$ 2.8 billion by 2030. But experts believe that the cost is, in fact, higher when considering the direct impact on individuals and households.
“Malaria hampers productivity and slows down the national economy as a result of illness and death to individuals. Therefore, the amount lost to this disease every year is surely more than what is being projected,” Peter Agadibe, a consultant pharmacist based in Lagos, said.
Professor of Paediatrics, and Strategic Adviser to Nigeria’s Minister of Health on Malaria Elimination, Olugbenga Mokuolu identified inadequate funding, health system weakness, including depletion of the workforce, insecurity, environmental challenges and behavioural patterns as some of the factors responsible for the country’s malaria crisis.
“We have issues with insecticide resistance, behavioural problems around inadequate use of available nets, poor diagnosis and [poor] treatment practices. While we have made progress on the fight against malaria, the challenge is that at any point in time, the resources deployed are a fraction of what is needed.
“The problem requires a multisectoral response, mobilising resources, and innovative approaches to improve access to preventive and treatment tools,” he said.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price





