Paris, France | AFP | “It’s magic,” said Francois, smiling. “Every time I take a pill I think about the people who aren’t so lucky as to have this option.”
Taking a drug normally prescribed to treat AIDS as a way to shield against the deadly disease — known as PrEP — is catching on, and proponents hope that it will soon have a measurable impact in reducing the number of infections.
“Besides its undeniable benefits for individuals, we need to know if PrEP confers a collective advantage too with a lower number of new cases,” said French expert Jean-Michel Molina ahead of World Aids Day on Friday.
There are nearly 20 million people around the world taking anti-retroviral therapy (ART) medication today, and another 17 million who need it.
HIV has infected 76 million people, and killed 35 million.
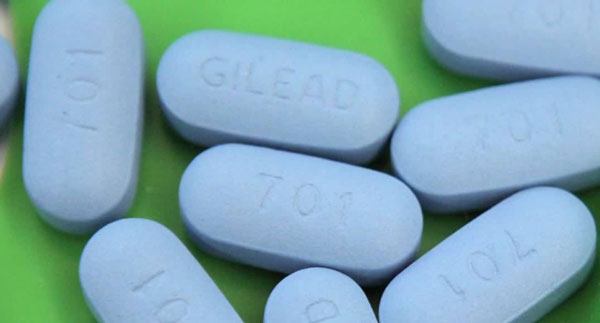
The idea behind PrEP — pre-exposure prophylaxis — is simple: high-risk persons who are HIV-negative take Truvada, normally prescribed to patients already infected, in order to prevent the virus from taking hold.
Target groups are men who have sex with men, and heterosexual couples in which one person is HIV-positive. The World Health Organization has also recommended that sex workers adopt a PrEP regimen.
The United States, in 2012, and France three years later were the first two countries to authorise this form of preventative treatment. Others have followed suit, including Canada, Kenya, Brazil, Thailand, Australia, Belgium, Scotland and South Africa, where 19 percent of the population live with HIV/AIDS.
– Seatbelts and airbags –
In France — the first country in which PrEP has available without cost — “about five in 10,000 people” should be taking it, said Molina.
So far, there has been no measurable effect: in 2016, France saw 6,000 new infections, the same level as for the last ten years.
“The number of people who have started PrEP — about 3,000 — is probably not enough to have had a statistical impact,” France’s public health watchdog agency concluded recently.
Prep can be taken regularly (one pill a day), or “as needed” before and after sexual encounters. But treatment protocols must be scrupulously respected to ensure protection.
“We don’t yet have a vaccine against AIDS, but PrEP is a new and effective form of prevention alongside condoms,” said Molina, who leads the ongoing Ipergay study for France’s AIDS Research Agency.
Francois, 55, is gay and lives in Paris. He has been on PrEP for 18 months. “The sword hanging over my head has vanished,” he said in an interview.
“The day one forgets a condom or it breaks, I no longer have that sick feeling in the pit of my stomach.”
In France, “PrEPers”, as they are called, are required to have blood tests every three months, in part to scan for other sexually transmitted diseases not blocked by the treatment.
PrEP is not without critics.
The main objection is that it encourages risky behaviour, including sex without condoms.
– Generics –
“It is important to protect against other STDs,” said Molina. “In a car, it better to use a seatbelt and have an airbag too.”
Francois says he “uses condoms with strangers,” but not with regular partners. “PrEPers who don’t use condoms at all probably didn’t use them before either,” he speculated.
Coverage of PrEP’s cost under public health insurance has also been criticised as tantamount to subsidising reckless sex.
“A doctor shouldn’t pass judgment, but rather protect health,” retorted Molina. “If PrEP helps to avoid infection, it has to be offered to patients.”
Besides, he added, taking the drug preventively cost less in the long run than treating HIV-positive patients for life.
The European patent for Truvada, made by US firm Gilead, expired at the end of July, bringing generics onto the market. As a result, the average price of treatment has dropped from 500 to 180 euros ($600 to $210).
PrEP is prescribed in Germany, but is not reimbursed. In England, health officials have recently recruited 10,000 volunteers for a three-year study to gauge it effectiveness.
“PrEP alone will not stem the epidemic,” said Molina.
“The three-pronged approach needed remains the same: treatment of HIV-positive patients, frequent testing of high-risk populations, and prevention, via condoms and now, PrEP.”
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price


