
There is urgent need to protect Ugandan health care workers in their line of duty
COMMENT | DR AMBROSE OTAU TALISUNA & DR DEOGRATIAS SEKIMPI | Infectious disease epidemics and pandemics (worldwide epidemic) continue to threaten the health of populations in Uganda and worldwide. In the past century, there have been four influenza pandemics that have claimed millions of lives. In addition, several new and old infectious diseases have emerged in new regions suggesting that humanity will continue to face future epidemics. Examples of large epidemics in Africa include HIV/AIDs, Cholera, Ebola Virus Disease, Marburg Virus disease, Malaria, Tuberculosis (both drug susceptible and drug resistant), and most recently, COVID-19 and Mpox. The COVID-19 pandemic is the greatest challenge that humankind has faced in generations – costing millions of lives, causing trillions of dollars in economic loss, and disrupting communities.
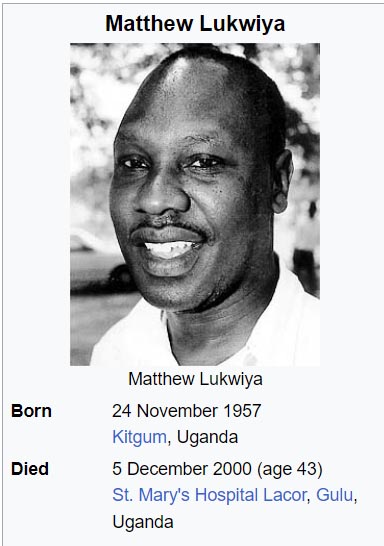
On 5th December 2000, Uganda lost Dr Matthew Lukwiya during the first Ebola Virus Disease (EVD) epidemic in the country. Many health care workers were lost over the period October 2000 to February 2001, many of them from Lacor hospital in Gulu district. All the lost health care workers are heroes but the leading hero for that response was Dr Mathew Lukwiya. In memory of Dr Mathew Lukwiya and other health care workers who have lost their lives in the line of duty, the Uganda National Association for Community and Occupational Health (UNACOH) has since 2002, held the annual Dr Mathew Lukwiya Memorial Lecture.
The UNACOH launched its first conference on 26th September 1987. However due to teething challenges the next conference did not take place until September 1993. Since then, except during the COVID-19 pandemic lockdowns in 2020, UNACOH has held annual scientific conferences.
The 2000 annual scientific conference was attended among others by a Master of Public Health (MPH) degree post graduate student-Dr Matthew Lukwiya. Shortly after, on the 8th of October 2000, a mysterious disease, later confirmed to be the first Ebola Virus Disease epidemic in Uganda was reported from Gulu District. Dr Lukwiya who had then completed his MPH degree but was in Kampala was the first to make the alarm about that Ebola virus disease epidemic.
He traveled from Kampala to Lacor Hospital where he swiftly set up an isolation ward for the treatment of Ebola cases. He also started educating Lacor Hospital staff about barrier nursing (as it was called then ) and infection prevention and control measures. He was one of three doctors who volunteered to work in the isolation ward from the start of the epidemic. His presence strengthened the response to the epidemic. Unfortunately, Dr Mathew Lukwiya contracted the disease and on the 5th of December 2000, he died, despite medical efforts and nation-wide prayers for God to spare his life. His last words were “ I am going to die now, I pray no one has to die of this disease again”.
 That Ebola Virus Disease epidemic was characterized by fever and bleeding manifestations and affected health workers and the general population of Rwot-Obillo, a village 14 km north of Gulu town. Later, it spread to other parts of the country including Mbarara and Masindi districts. The epidemic lasted up to the 16 January 2001 and a total of 425 cases with 224 deaths ( case fatality of 53%) were reported countrywide. Thanks to the efforts of our heroes, the epidemic was declared over on the 27 February 2001.
That Ebola Virus Disease epidemic was characterized by fever and bleeding manifestations and affected health workers and the general population of Rwot-Obillo, a village 14 km north of Gulu town. Later, it spread to other parts of the country including Mbarara and Masindi districts. The epidemic lasted up to the 16 January 2001 and a total of 425 cases with 224 deaths ( case fatality of 53%) were reported countrywide. Thanks to the efforts of our heroes, the epidemic was declared over on the 27 February 2001.
From the 16th-18th of October 2024, the 18th Joint Annual Scientific Health (JASH) conference, the 30th UNACOH conference and the 8th Uganda Medical Association (UMA) Grand Doctors Conference (GDC) and Annual General Meeting (AGM) will be held, culminating in the 22nd Dr Mathew Lukwiya Memorial Lecture.
The theme for this year’s conference, to be held at Hotel Africana in Kampala Uganda, is “Global Health Security: Partnerships for Epidemic Response and Control in sub-Saharan Africa”. This year’s Dr Mathew Lukwiya lecture will be delivered on the 18th of October 2024 and is titled “Global Health Security: The urgent need for expanding partnerships and protecting frontline health workers”.
The World Health Organisation (WHO) defines Global Health Security as “the activities required, both proactively and reactively, to minimize the vulnerability to any public health emergencies that endanger the collective health of populations living across geographical regions and international boundaries. Health security becomes a general security and development concern when it threatens a nation’s ability to function and safeguard its citizens’ welfare, including provision of basic services. The rapid spread of the COVID-19 pandemic demonstrates this new critical concern. It also necessitates the adoption of a holistic approach to health, reflecting both a health security approach (controlling the health emergency) and a health development approach (tackling upstream causes and determinants).
Although investments in health security are crucial, including early warning systems and laboratory networks, adequate health work force and adequate clinical care, health security alone is not sufficient because it leads to verticalizing infectious disease prevention and control, often overlooking the broader health systems that are chronically underfunded, fragmented, under resourced and inequitable. The COVID-19 pandemic has brought to the surface the crucial relationship between health system capacities and effective health security response.
In most countries, health system deficiencies hindered effective response. These include a lack of emergency planning and leadership, inadequate health work force, shortages of infrastructure and equipment, disruptions to medical supply chains, limited scale-up capacity to respond to increases in caseloads, inadequate information on health systems capacities, as well as a weak engagement of the private sector providers with governments in national pandemic responses.
The sad reality is that there can be no genuine and resilient global health security system without strong and resilient health systems with fit for purpose essential public health functions and adequate resources at all levels. Health systems that can effectively leverage both robust global health security core capacities – for instance risk communication, surveillance, and laboratories – and fundamental universal health coverage interventions such as primary health care, accessible health facilities, health worker force and affordable medicines and supplies, are in a better position to protect their citizens against the social and economic impacts of the epidemics and pandemics.
During epidemics we often witness disruptions to many programmes including those for maternal and child health, communicable disease control, routine immunization, and non-communicable disease control. These disruptions are largely attributed to inadequate progress on universal health coverage and limited consideration for the role of primary health care in preparedness and response to epidemics. Thus, overall health outcomes are unlikely to improve without simultaneously addressing both universal health coverage and global health security. Thus, mobilizing investments in a health system approach therefore represents a “double-win”.
Dr Matthew Lukwiya has been and continues to be a symbol that represents all health care workers who have lost their lives in the course of saving the lives of other Ugandans. The COVID-19 pandemic gives further significance to this year’s Dr Lukwiya Memorial lecture in view of the numbers of health care workers that have lost their lives because of inadequate capacities in their work environment.
In closing, the role of our health care workers is to save lives and alleviate the suffering of patients. It is NOT to get infected and die because of poor working environments and limited capacities to Prevent, Detect and Respond to epidemics.
We call upon the government and Uganda’s development partners to act now to stop health care workers infections and deaths in line of duty. In this, the government, development partners, the public (community), and the health workers need to speak with one voice, and act in unison, to ensure that all Ugandans come out as winners.
******
 ✳Dr Ambrose Otau Talisuna is a Ugandan medical doctor, epidemiologist, and public health expert in global health based in Addis Ababa, Ethiopia. He has expertise and experience spanning close to 30 years in Uganda and internationally in health emergency preparedness and response, international health regulations, integrated disease surveillance and response, communicable disease prevention and control, malaria control and elimination, health information systems, health systems strengthening and evaluation. Dr Talisuna will deliver the 2024 Dr Mathew Lukwiya Memorial Lecture.
✳Dr Ambrose Otau Talisuna is a Ugandan medical doctor, epidemiologist, and public health expert in global health based in Addis Ababa, Ethiopia. He has expertise and experience spanning close to 30 years in Uganda and internationally in health emergency preparedness and response, international health regulations, integrated disease surveillance and response, communicable disease prevention and control, malaria control and elimination, health information systems, health systems strengthening and evaluation. Dr Talisuna will deliver the 2024 Dr Mathew Lukwiya Memorial Lecture.
✳Dr Deogratias Kaheeru Sekimpi is a Ugandan medical doctor, public health and occupational health expert, who has promoted the health and safety of health care workers over the years. He liaised with the World Health Organization (WHO) and Uganda National Association of Community and Occupational Health (UNACOH) to initiate the annual Dr Mathew Lukwiya Memorial Lecture in 2002, and still supports it perpetuation to-date. Formerly President, and Executive Director, of UNACOH, Dr Sekimpi is now the inaugural Secretary General of the East, Central and Southern Africa College of Public Health Physicians (ECSA-COPHP).
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



