The burden of post-TB lung disease and the health and well-being of TB survivors is poorly understood
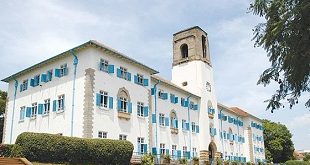
Kampala, Uganda | PATRICIA AKANKWATSA | The National TB and Leprosy Programme at the Ministry of Health, Makerere University Lung Institute and the Global Fund have partnered to implement an innovative programme focused on affordable and accessible post- TB Lung disease (PTLD) assessment and care.
Uganda is among the 22 countries with the highest TB burden, with an estimated incidence of 200 cases per 100,000. Collaborative efforts have led to significant progress in TB treatment, benefiting over 500,000 Ugandans since 2015. Treatment success rates have improved from 72% in 2015 to 84% in 2022, underscoring the impact of ongoing interventions.
According to the World Health Organisation (WHO) reports, about 74 million lives were saved through tuberculosis (TB) diagnosis and treatment between 2000 and 2021.
Despite emerging evidence, there is still a lack of international guidelines and recommendations on the follow-up of patients beyond the cure of TB. While WHO’s Global Action Plan on non-communicable diseases recommends incorporating screening for chronic respiratory disease in TB clinics, the WHO End TB Strategy neglects post-TB respiratory disorders.
Currently, health systems, especially in Africa, do not recognise that TB care extends beyond treating the initial infection, which leaves the majority of survivors at a higher risk of both clinical and socio-economic consequences even after a microbiologic cure of TB.
In Uganda, the burden of post-TB lung disease, and the health and well-being of TB survivors is poorly understood partly because of a lack of literature, and this contributes to poor health service provision in this subpopulation.
This was revealed at the two-day Tuberculosis and Leprosy Summit held in Kampala on March 19-20 under the theme: “Harnessing Local Research and Innovation on TB and Leprosy to Shape National Policy and Practice to End & Leprosy in Uganda”
Dr Henry Luzze who is the deputy director of the programme says that while successful TB treatment eliminates the active bacteria, lung damage can persist, leading to PTLD.
“TB and its treatments can leave a person with permanently damaged tissues,” he said adding that: “Many survivors also experience ongoing psychosocial and economic effects, which also need to be addressed as part of a system-wide approach to improving survivors’ quality of life”.
Survivors typically experience a transition from acute illness to living with multifaceted chronic disease. Post-TB morbidity affects adults and children and varies widely. It can include physical conditions such as PTLD, which has been defined as a chronic respiratory abnormality partially attributed to previous pulmonary TB.
“Even after defeating TB, many survivors face a daily struggle for breath due to PTLD,” said Luzze.
He said TB survivors have up to three times increased risk of mortality from post-pulmonary TB lung complications compared with the general population, with a prevalence of lung impairment between 18% and 87%.
He adds that Delayed diagnosis and inappropriate regimens used during treatment may play a role in the development of PTLD.
“Former TB patients experience increased non-pulmonary morbidity and mortality, particularly cardiovascular diseases, despite successful completion of treatment,” he said.
Geoffrey Amanya an epidemiologist at Makerere University’s Lung Institute, said there are plenty of missed opportunities from their surveillance system to capture for PTLD associated factors and diagnosis and treatment.
“We need routine monitoring and treatment of PTLD to be implemented in various programmatic settings,” he said.
Research from Makerere Lung Institute shows that 50% of TB survivors have PTLD and that 9.5% of deaths occurred between 2020 and 2023 because of PTLD.
Mudarshiru Bbuye also an epidemiologist at the Makerere Lung Institute and one of the researchers on the project says that this programme will reduce the risk of morbidity and mortality due to post-TB impairments following TB cure and completion
“This package empowers patients to actively manage their PTLD. By learning proper breathing techniques and understanding their condition, they gain control over their well-being and minimize the impact of PTLD on their daily lives,” he said.
The Global Fund’s financial contribution plays an important role in scaling up this initiative. “The grant allows us to train healthcare workers at all levels, from primary care physicians to community health workers,” explains Dr Luzze.
“This not only expands program reach but also equips healthcare providers nationwide with the necessary skills to effectively identify and manage PTLD,”
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price