
African health experts call for African solutions
NEWS ANALYSIS | RONALD MUSOKE | When health ministers from nine African countries held an emergency meeting in Kampala on Oct.12, they had one goal; to prevent any cross-border spillover of the Ebolavirus disease that was confirmed almost a month ago in central-western Uganda.
The current outbreak has affected five districts neighbouring the epicentre, Mubende, and as of Oct.17, there were 60 confirmed cases, 24 deaths and 20 other probable Ebola-related deaths reported by the Ministry of Health.
Following an intensification of response from the government with help from the World Health Organisation (WHO) and other agencies, more than 1500 contacts have been identified, while 24 people including five medical personnel have recovered from the disease.
Although the government in Uganda says the Ebola crisis is under control and continues to appeal for calm, outside the country, everyone seems worried.
The U.S. government said Oct.6 it would with immediate effect start directing travellers who had spent time in Uganda to five airports (New York’s JFK, Newark, Atlanta, Chicago O’Hare and Washington Dulles) for health screening before entering the country.
Uganda’s immediate neighbours including Kenya, Tanzania and South Sudan also heightened their screening protocols for visitors coming from Uganda. On Oct.12, the World Health Organisation announced it urgently needs support to prevent the Ebola outbreak from spilling over into the neighbouring countries.
“Our primary focus now is to support the government of Uganda to rapidly control and contain this outbreak, to stop it from spreading to neighbouring districts and neighboring countries,” WHO Director General, Tedros Adhanom Ghebreyesus, said Oct.12 in Geneva, Switzerland.
Dr. Mike Ryan, the head of the WHO’s health emergencies programme, said Oct.12 that Uganda’s government needs more support from the international community to ramp up surveillance on the ground to contain the outbreak. Ryan said not enough health alerts are being issued at the local level.
“We are seeing good progress,” Ryan said. “It’s very important that we are not confident. Ebola brings surprises, infectious disease brings surprises.”
I would like to appreciate @WHO, @WHOAFRO, @WHOUganda, @AfricaCDC, @_AfricanUnion and all our collaborating partners for supporting this meeting and our overall response to the #EbolaOutbreakUG.
Strong partnerships and collaboration are the cornerstone of any response. pic.twitter.com/Bwvvyv2gpA
— Dr. Jane Ruth Aceng Ocero (@JaneRuth_Aceng) October 12, 2022
Kampala emergency conference
At the Kampala meeting, Dr Ahmed Ogwell Ouma, the Acting Director General of the Addis Ababa-based Africa Centres for Disease Control and Prevention, said although the Mubende outbreak is the eighth epidemic of the Sudan strain of Ebola in Africa, there is no vaccine for it yet. He said it is unfortunate that there are no rapid diagnostics for this strain of the virus and no vaccines for it.
“The reality for us is that when a public health crisis is big, like the COVID-19 pandemic, Africa is on its own as the rest of the world produces and uses their own health products while we find ourselves at the end of the queue,” he said.
“When an outbreak is smaller and affects only Africa – like Ebola, Lassa fever, and monkey pox – then Africa is still on its own.” Dr. Ouma said African epidemics seem to attract urgent attention when the transmission crosses the shores of Africa and affects other parts of the world.
“Africa must now do things differently; knowing that we are on our own must be the motivating factor for us to do things on our own, but not alone because the world is now literally one,” he said.
“We must learn from ourselves and others; we must plan, prepare and respond effectively using our local resources including our experts and institutions; and we must produce the health products we have identified as a priority for Africa.”
Dr. Ouma noted that in spite of the African countries dedicating immense resources to bring these outbreaks under control, it is now clearer that controlling these diseases will require a sustained and new way of working.
“We are meeting to build on our existing experiences and collaborations within the region and beyond. This is because in our increasingly interconnected world, diseases know no borders,” he said.
He said, drawing on lessons from the 2014–2016 Ebola outbreak in West Africa, and the current COVID-19 pandemic, it’s evident that preparedness for and response to disease threats is not just a technical matter but also a very serious economic and political matter.
He said it requires each country to make a contribution and make Africa safer and better. Dr Ouma noted that a proactive approach to public health emergencies is what is now needed.
“The International Health Regulations (2005) are anchored on governments being accountable to both their citizens and the international community in managing outbreaks, and we are therefore obliged to develop a set of core public health capacities to detect, assess, and respond to infectious disease emergencies,” he said.
The ministers agreed in a communiqué on joint measures to stop the potential spread of the ongoing Ebola disease outbreak in Uganda and beyond its borders. The ministers also agreed on ensuring joint cross-border readiness and rapid cross-border deployment of medical personnel to tackle the disease, and public awareness and community engagement campaigns.
Building an Ebola firewall
The Kampala meeting followed an assessment by WHO which found the risk of the Ebolavirus outbreak spreading to neighbouring countries quite high due to cross border movements between Uganda and other countries.
“One of the crucial lessons Africa has learnt from previous Ebola outbreaks is that by uniting, we stay a step ahead of the virus. Through sharing information and resources, countries can go from firefighting to building an outbreak firewall and halting the spread of infections,” said Dr Matshidiso Moeti, the WHO Regional Director for Africa.
Dr. Ouma also emphasised the need for collaboration in ensuring health security of the Eastern Africa region and beyond.
“We as a continent must work together to plan, prepare and respond to the Ebola outbreak and other public health threats through resource sharing, regional efforts to build resilience capacity of human resources, strengthen laboratory systems, surveillance, treatment and care,” he said.
Ebola epicentre
The epicentre of the latest Ebola outbreak in Uganda lies about 150km to the west of Kampala. But it is along the busy “Northern Corridor Road” which connects the Indian Ocean Kenyan port of Mombasa to the eastern African hinterland (Uganda, Rwanda, Burundi, eastern Democratic Republic of the Congo and northern Tanzania).
Mubende District also hosts several gold mines, which have in recent years attracted people from different parts of Uganda, as well as neighbouring countries. The population is mobile due to trade, social and cultural connections.
But also Uganda hosts many refugees who are mainly from South Sudan and the Democratic Republic of Congo. These refugees continue to keep ties with their countries of origin. It is these trade, social and cultural connections that government officials say, have posed a challenge in managing this highly infectious hemorrhagic disease.
Ebola is a severe, often fatal illness affecting humans and other primates. It has six different types, three of which (Bundibugyo, Sudan and Zaire) have previously caused large outbreaks on the continent.
The virus is spread by contact with bats and monkeys and also by contact with a person infected by the Ebola virus. It spreads quickly from person to person, kills in a short time but death can be prevented; especially if it is detected early and patients are put on treatment.
A person suffering from Ebola presents symptoms including; high fever (brutal and prolonged), abdominal pain, joint or body pain (especially the chest, difficulty in swallowing, headache, nauseas, vomiting (can be bloody), diarrhoea (can be bloody), dehydration (no tears, dry tongue, sunken eyes) and rash. In other cases, there can be bleeding from the mouth, eyes, nose, ears, and anus.
Uganda’s seventh Ebola outbreak
On Sept.20, Uganda declared an outbreak of Ebola (Sudan type) after a case was confirmed in a village in Madudu sub-county in Mubende District. According to the Ministry of Health, the first case was that of a 24-year old man who developed a wide range of symptoms on Sept.11 including high-grade fever, tonic convulsions, blood-stained vomit and diarrhoea, loss of appetite, pain while swallowing, chest pain, dry cough and bleeding in the eyes.
The young man visited two private clinics, successively from Sept.11-15 without improvement. He was then referred to Mubende Regional Referral Hospital on Sept.15 where he was isolated as a suspected case of viral haemorrhagic fever.
A blood sample was collected on Sept.17 and sent to the Uganda Virus Research Institute (UVRI) in Kampala where RT- PCR tests were conducted and returned positive on Sept. 19. On the same day, the patient died.
#WHO strengthens the capacities of 15 Healthcare workers on #Ebola case management in Kyegegwa district. Activities include Screening and Triage, Isolation of suspected cases, Hand hygiene, proper use of Personal Protective Equipment when caring for #Ebola patients. pic.twitter.com/e2iOpBDiRa
— WHO Uganda (@WHOUganda) October 17, 2022
Meanwhile, results of preliminary investigations identified a number of community deaths from an unknown illness in Madudu and Kiruma sub-counties in Mubende in the first two weeks of September. These deaths are now considered to be probable cases of Ebola.
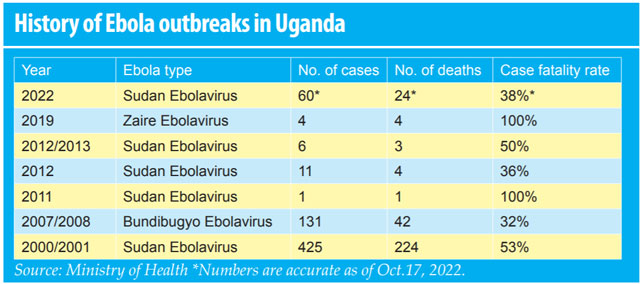
Before this year’s outbreak in Mubende District, there were six Ebola incidents reported in the country since the turn of the millennium in 2000. The first ever reported outbreak occurred in the northern district of Gulu in 2000, followed by Bundibugyo in 2007, Luweero in 2011, Kibaale in July 2012, and Luweero in November 2012. There was also a spillover from DR Congo reported in Kasese District in June 2019.
In total, Uganda’s Ministry of Health records show that 638 people have been infected over the last two decades with at least 300 deaths. Of these seven outbreaks, five were from the Sudan strain and one each from the Zaire and Bundibugyo types.
But Dr. Jane Ruth Aceng, Uganda’s Minister of Health noted at the Kampala meeting that given the fact that Uganda has battled repeated outbreaks of viral hemorrhagic fevers; the country has developed some capacity to deal with such epidemics.
There has, for instance, been a well-coordinated response to these epidemics led by a multi-sectoral National Task Force under the leadership of President Yoweri Museveni and the Office of the Prime Minister.
“Uganda is alive to the fact that community engagement is very important for outbreak control; epidemics begin and end in communities,” Dr. Aceng said, “When communities are engaged and trained in epidemic preparedness and response, they can find and stop outbreaks which will ultimately save lives, restore services and helps build resilience.”
Dr Aceng also praised the country’s capacity in laboratory testing of Ebola. All tests, the minister said, are done within the country. In fact, for this particular out-break; in order to cut the result turnaround time, the government with the help of the World Health Organisation has deployed a state of the art mobile Lab at the epicentre of the outbreak, and this has reduced the turnaround time for results to just six hours.
But, as Dr. Aceng was singing the government’s praises for handling of the latest outbreak, there has also been some muffled criticism thrown in the direction of the government. The critics cite alleged haphazard community engagement and community-based surveillance which, by Dr. Aceng’s own account, is critical in any response.
One month into the outbreak, it remains unclear how and when exactly epidemic began. Critics also point to some poor coordination between the village health teams and the surveillance teams at sub-county and district levels.
There also appears to be a lack of trust between the communities in Mubende and the health authorities. Convincing Ebola suspects to go to the designated quarantine centres has at times been a struggle; with most of the suspected cases instead choosing to be treated by traditional healers in their communities.
One of the bizarre incidents happened at the beginning of this month when a 45-year-old man who was a known contact under follow-up escaped from his home in Kanseera village, Kirwanyi Parish, Kiruuma Sub-county in Mubende, travelled a distance of over 170km to Luweero District, in central Uganda, to seek treatment from a traditional healer.
When his condition deteriorated on Oct.06, he travelled another 60km to Kiruddu National Referral Hospital in Kampala from where he reportedly died on Oct.7.
Ministry of Health surveillance teams had on Sept.23 listed this man as a contact person to his 18-year old brother who died of Ebola at Mubende Hospital. He was being followed up but disappeared from his residence. It is reported that on Oct.3, his condition deteriorated and he was taken by his family to a traditional healer in Luweero District.
At Kiruddu Hospital, the man later identified as Twagiira Yezu Ndahiiro gave wrong names and address to divert the health workers’ attention from associating him with the ongoing Ebola outbreak in Mubende.
The health workers at Kiruddu suspected him to have liver/kidney problem and peptic ulcers. The health workers, however, used protective wear while attending to him. He died 10 hours later. But even when the relatives knew the truth, they asked for his body which they transported back to his village in Kanseera, Mubende District, on top of a public taxi.

The Mubende District security teams tried to intercept the commuter taxi that carried the body but they apparently failed to halt it. Later, they found the family and intervened to have a supervised burial conducted by the certified burial teams in Mubende, President Yoweri Museveni said, during his second update on the Ebola outbreak on Oct.12.
Museveni said a sample from the deceased was later taken off by the burial team, tested the same day and returned positive for Ebola.
Interestingly, Twagiira Yezu’s family had previously not been cooperative following suspected death in their family. On Oct.1, the family apparently hijacked a dead body of a confirmed Ebola case and performed traditional burial rituals, in total disregard to the SOPs for managing dead bodies of confirmed cases.
This same family also hid a confirmed Ebola case, a 49 year old male who later died on Oct.10 shortly before the surveillance teams got to them and quarantined them. The family has so far lost 10 people to Ebola.
President Yoweri Museveni said the behaviour exhibited by this family of refusing follow up, running away to look for treatment at the traditional healer’s shrines, telling lies and hijacking dead bodies of Ebola cases for rituals posed a great risk of spreading Ebola to the communities and the surrounding districts.
“We cannot allow this to go on because it puts the lives of all Ugandans at risk and disrupts normal activities in the area and the entire country,” he said.
“This family must cooperate with the district officials and health workers. They should stop moving around seeking treatment from witch doctors. I am happy that majority are under quarantine.”
“Those who ran away should come back for close observation so that if they fall sick, treatment can be started early. Those who are in hiding should come out immediately and report to the health workers for proper follow up,” Museveni said.
The surveillance security teams have since searched and picked up to 15 contacts including the late Twagira Yezu’s family and neighours for quarantine.
In his televised address on Oct.12, President Museveni said, the communities in the affected districts should understand that Ebola disease is deadly and spreads through contact with someone who has symptoms.
“When you see somebody with symptoms or if you develop symptoms, call the health workers to take you to the health facility in their ambulances,” he said, “Do not jump on a boda boda or a taxi because you will spread the infection to the ones transporting you. The health workers must use appropriate protective wear (gloves, aprons, masks) whenever they are examining patients.”
He also directed traditional healers, herbalists and religious leaders to stop accepting sick people with symptoms of Ebola in their shrines or worship seeking for treatment or prayer, respectively.“Advise them to call health workers for safe transfer to hospitals,” Museveni said.
Museveni also wants the security teams supporting the response teams in the districts to be “very vigilant” and ensure no Ebola patients in treatment centres or contacts in the quarantine facilities escape.
‘No Ebola in Kampala’
Even when there have been rumours circulating on social media platforms of sick people presenting with Ebola-like symptoms in some health facilities including Kiruddu Hospital, Museveni concluded his address by reiterating the official government position saying there is no Ebola in Kampala.
He said the only confirmed case was that of Twagira Yezu who came from Mubende via Luweero and was admitted at Kiruddu Hospital and died. But Museveni quickly added that the Twagira Yezu case
shows the possibility of Ebola erupting in Kampala if there is no vigilance and people remain defiant to medical advice.
Museveni said many people have been reporting with signs and symptoms similar to Ebola within Kampala and Wakiso over the last few weeks but these so-called “alert cases” that have been tested have all returned negative results.
That was on Oct.12. A day later, on Oct.13, the situation changed. A new case was reported, in a small city health facility at Kitebi, in the western division of Rubaga.
Dr. Aceng, the Health minister, was back on social media to calm the nerves of the public, especially those living and working in Kampala. The new case, the minister said, was that of the wife of the case who went to Luweero and ended up at Kiruddu and passed on (Twagiira Yezu).
“She is a listed contact of her husband’s brother before that. She was listed as contact in Mubende therefore she remains a case of Mubende,” Dr. Aceng said.
“She tested positive on Oct.13 after delivery and she is currently in isolation at the facility in Entebbe. The health workers who attended to her are also in quarantine at Mulago isolation facility and will be under watch for the next 21 days.”
“I want to state very clearly that this does not mean that Kampala has Ebola. Cases that were already listed in Mubende remain cases of Mubende. Until Kampala generates its own cases that start within Kampala, we cannot call that a Kampala case,” the minister said.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price



