New research shows what must be done about it
| THE INDEPENDENT | Early diagnosis is crucial for the effective management of any disease. In Africa, this is not always possible which affects the ability of countries to bring diseases under control.
Wilber Sabiiti, a Senior Research Fellow in Medicine, University of St Andrews, UK, and colleagues conducted research into the barriers to diagnosis for tubercolosis (TB) in Kenya, Tanzania and Uganda. They also wanted to identify what opportunities there were to maximise the use of diagnostics in healthcare settings.
According to the researchers, the COVID-19 pandemic has led to an unprecedented uptake and utilisation of molecular diagnostics worldwide with over 500 million tests conducted in a period of 9 months by October 2020.
They say health systems have been shaken but most importantly the pandemic has raised public consciousness of the value of diagnostics and interdisciplinary approaches in the control of diseases.
In contrast, tuberculosis (TB) has been a pandemic for time immemorial and a global public health emergency for over 20 years. But the rate of TB testing does not match incidence of TB disease and, consequently, an estimated 3 million cases go undetected every year.
A quarter (1.7 billion) of the world population has TB infection and in 2018, 10 million developed active disease resulting in 1.5 million deaths. Of the 10 million notified cases, 55% were bacteriologically confirmed and a small proportion of these were tested using rapid molecular tests.
The World Health Organisation (WHO) approved routine use of TB molecular tests more than 10 years ago, starting with the Line Probe Assay (LPA) in 2008 and Xpert Mycobacterium tuberculosis/rifampicin (MTB/RIF) in 2010.
The Xpert MTB/RIF detects both TB and resistance to rifampicin in two hours and is the widely used molecular test for TB. But by 2016, only 16 million Xpert MTB/RIF tests had been performed, translating into 3.2 million tests per year.
The researchers found that, in Kenya, Tanzania and Uganda, the uptake of diagnostics had an urban rural divide. It was highest – over 90% – at large referral hospitals in major municipalities and cities, what they call “tertiary level health care facilities”. Meanwhile, lower level health care facilities, where most people live, were less served by diagnostic tests.
The study was completed prior to emergence of COVID-19. But a similar trend of over concentration of diagnostics in major cities has been repeated in COVID-19 responses in all the three countries.
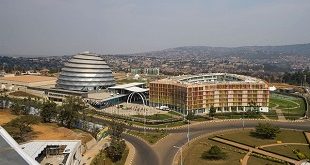
For instance, in Kenya 26 out of 47 COVID-19 PCR (polymerase chain reaction) testing laboratories are in Nairobi, while in Uganda 17 out of 22 are in Kampala. Until recently Tanzania had one national testing laboratory in Dar es Salaam. Five more laboratories have been approved for PCR testing.
This raises the question of the extent to which COVID-19 testing has been accessed by the rural communities of the three countries.
From their research, we concluded that each country needed to pursue solutions to unlock barriers to increase access to diagnostics.
The scientists says because there is sharp contrast in the rate of uptake of COVID-19 molecular tests compared with TB, a leaf could be borrowed from either disease on how to accelerate and maximise translation of health research innovations into policy and practice.
Countries must be encouraged to distribute essential healthcare provision – like diagnosis – to where people most need them and where they can be accessed more easily.
In addition, solutions must include increased domestic financing to improve healthcare at primary healthcare level; mass education to increase awareness of the available diagnostic and treatment tools and investing in community empowerment solutions.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price